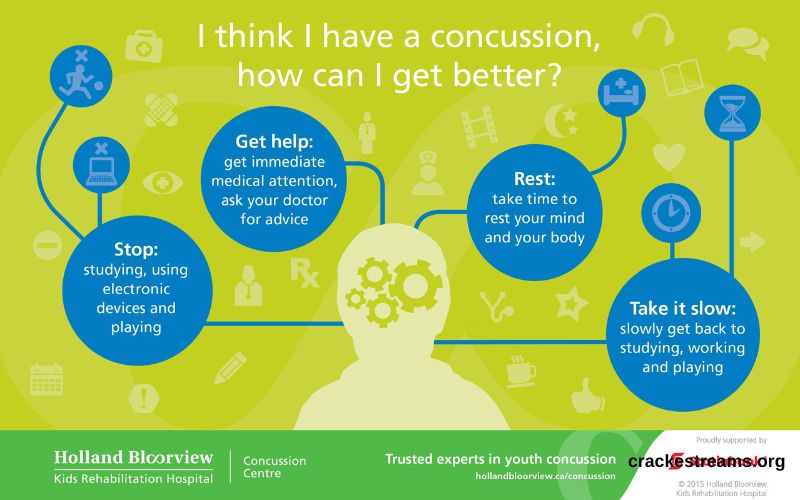
Recovery, a form of mild traumatic brain injury, can significantly impact an individual’s daily life. They result from a blow to the head or a sudden jolt that causes the brain to move within the skull, leading to various symptoms like headaches, dizziness, confusion, and more. Recovery from a concussion is a carefully monitored process that can be broken down into six distinct stages. This article will provide an in-depth look at each stage of concussion recovery, offering guidance on what to expect and how to manage the process effectively.
Stage 1: Immediate Post-Injury (24-48 Hours)
Objective: Rest and Initial Assessment
The first 24 to 48 hours following a concussion are critical for initial healing and assessment. During this time, the primary objective is to rest and limit activities that could exacerbate symptoms.
- Complete Rest: The brain needs time to start the healing process. This means avoiding physical and cognitive activities such as reading, watching TV, using electronic devices, and any physical exertion.
- Symptom Monitoring: Close monitoring of symptoms like headaches, nausea, dizziness, and sensitivity to light and noise is essential. Any signs of severe symptoms, such as worsening headaches, repeated vomiting, or loss of consciousness, require immediate medical attention.
- Medical Evaluation: A healthcare professional should perform a thorough evaluation to confirm the concussion and rule out more serious injuries like skull fractures or internal bleeding. This evaluation typically includes a neurological examination and may involve imaging tests if necessary.
- Hydration and Nutrition: Maintaining proper hydration and a balanced diet can support the body’s natural healing processes.
Stage 2: Acute Recovery (2-7 Days)
Objective: Gradual Reintroduction of Light Activities
In the acute recovery phase, which spans from the second day to about a week post-injury, the focus shifts to gradually reintroducing light activities while still prioritizing rest.
- Light Cognitive Activities: If symptoms have started to improve, individuals can engage in light cognitive activities such as listening to music, engaging in light conversations, or doing simple household tasks.
- Activity and Rest Balance: It’s important to balance activity with plenty of rest. Any activity that triggers or worsens symptoms should be stopped immediately.
- Avoiding Symptom Triggers: Bright lights, loud noises, and other potential symptom triggers should still be avoided during this phase.
- Continued Symptom Monitoring: Ongoing monitoring of symptoms is crucial. If symptoms worsen with activity, it indicates the need for more rest.
Stage 3: Return to Light Cognitive Activity (1-2 Weeks)
Objective: Gradual Resumption of Cognitive Tasks
By the end of the first week and moving into the second week, many individuals can begin returning to more structured cognitive activities.
- Short Cognitive Sessions: Engage in brief periods of cognitive tasks such as reading, writing, or working on a computer. It’s essential to keep these sessions short and take frequent breaks.
- Controlled Environment: Working in a quiet, controlled environment with minimal distractions helps manage symptoms. Avoiding overstimulation is key during this phase.
- Symptom-Limited Activity: Activities should remain symptom-limited. If symptoms worsen, the activity should be stopped immediately.
- Gradual Increase in Cognitive Load: Slowly increase the cognitive load as tolerated. If symptoms do not worsen, progressively extend the duration and complexity of tasks.
Stage 4: Return to School or Work (2-4 Weeks)
Objective: Gradual Return to Regular Academic or Work Activities
During the third and fourth weeks post-injury, the goal is to gradually return to academic or work responsibilities.
- Modified Schedules: Return to school or work on a modified schedule if needed, such as half-days or reduced workloads. This helps ease the transition back to full activity.
- Accommodations: Request accommodations such as extra breaks, reduced screen time, or a quieter workspace to help manage symptoms.
- Gradual Increase in Workload: Gradually increase the workload and complexity of tasks as tolerated. It’s important to avoid overexertion.
- Regular Monitoring: Regular check-ins with healthcare providers are important to track progress and make any necessary adjustments to the recovery plan.
Stage 5: Return to Light Physical Activity (3-5 Weeks)
Objective: Gradual Resumption of Light Physical Exercise
As cognitive activities are better tolerated, the focus shifts to reintroducing light physical activities.
- Light Aerobic Exercise: Engage in light aerobic activities such as walking, light jogging, or stationary cycling at a low intensity. These activities should be symptom-limited.
- Gradual Progression: Gradually increase the intensity and duration of physical activity based on tolerance. Start with short sessions and slowly build up.
- Avoiding High-Risk Activities: Avoid contact sports and activities that carry a high risk of head impact or heavy physical exertion until full recovery.
- Symptom Monitoring: Regularly monitor symptoms during and after physical activity. If symptoms worsen, reduce the intensity and duration of exercise.
Stage 6: Full Return to Normal Activities (5-6 Weeks and Beyond)
Objective: Full Return to Academic, Work, and Physical Activities
The final stage involves a full return to normal academic, work, and physical activities. The individual should be symptom-free at rest and during exertion.
- Return to Sport: For athletes, follow a step-by-step return-to-play protocol under medical supervision. Each step should be completed without symptoms before progressing to the next.
- Full Academic and Workload: Handle a full academic or work schedule without accommodations. Cognitive and physical tasks should no longer trigger symptoms.
- Ongoing Monitoring: Continue to monitor for any recurring symptoms and seek medical advice if they reappear.
- Long-Term Management: Some individuals may experience prolonged or persistent symptoms. In such cases, a comprehensive management plan involving multidisciplinary care, including neurology, psychology, and physical therapy, may be required.
Additional Considerations
Psychological Support
The emotional and psychological impact of a concussion can be significant. Feelings of frustration, anxiety, and depression are common, particularly if the recovery is prolonged. Seeking support from mental health professionals, such as psychologists or counselors, can be beneficial.
Education and Awareness
Educating patients, families, coaches, and teachers about concussions and their management is crucial. Understanding the importance of each stage of recovery and recognizing the signs of worsening symptoms can help prevent further injury and promote a smoother recovery.
Prevention Strategies
Preventing future concussions involves wearing appropriate protective gear during sports, following safety rules, and creating environments that minimize the risk of head injuries. Raising awareness about the risks and symptoms of concussions can also contribute to better prevention and management.
Conclusion
Concussion recovery is a multi-stage process that requires careful management and a gradual return to normal activities. Each stage is designed to allow the brain to heal while minimizing the risk of further injury. By following these stages and working closely with healthcare providers, individuals can maximize their chances of a full recovery and a return to their regular routines. Education, awareness, and support are key components in navigating the journey from concussion to recovery.
Understanding and adhering to the six stages of concussion recovery is crucial for ensuring a safe and effective healing process. By taking the necessary precautions and following medical advice, individuals can successfully navigate their recovery and return to their normal activities with confidence and health.